OK, I got a question here that came in from our Pediatric Direct Care Summit.
I just wanted to talk through it because it’s a common question that comes up around boundaries in pediatric direct care.
One of the things that makes it challenging in pediatric direct care is that a lot of the care we provide is relatively easy and non-burdensome. That eight o’clock text message that comes in wondering about potty training probably doesn’t take a lot for me to take a moment to answer.
Now, it would certainly break my boundary of not answering text messages after hours to do so. Even though it would be relatively easy—maybe just a few quick sentences or thoughts—it does pull me away from my family, my recharging, my evening, whatever I might be doing.
There are lots of opportunities for boundaries to get tested and broken in pediatric direct primary care because much of what we do is relatively easy to provide and feels like a big win for families.
For example:
“It’s 9 o’clock and my child has this barky cough. What should I do?”
In a typical practice, you’re on your own until morning. Maybe there’s a nurse triage line. Maybe you go to the ER because urgent care is closed.
In direct care, it’s tempting to say, “What if I just run over a dose of Decadron to your home at 9 o’clock, or 2 AM, or Sunday afternoon?”
Those are all things you can do. But the question is: how do I set boundaries for established patients when I’ve been overly accommodating so far?
You don’t want to spend your career getting up at 2 AM to give a little Decadron to a child across town. And you don’t need to.
Why Boundaries Matter
I think that’s one of the things that keeps pediatricians from going into direct care:
Feeling like they’ll be on call all the time
Feeling like patients will be demanding (“I’m paying for this, I should get carte blanche”)
But patients realize, as you build a relationship, that you’re a human being too. You’re not available at all times, nor should they expect that—especially at the price points we’re talking about.
This isn’t the $10,000 per month, helicopter-to-your-home-in-the-Hamptons model. This is pediatric direct primary care.
Step 1: Decide Internally
When you want to reset your boundaries, the first thing is to decide internally what those boundaries are.
You may have had experiences where you thought:
“That was outside my boundaries.”
“I did it this time, but if it became a systemic habit it would wear me down.”
Sometimes you will intentionally adjust your boundaries.
Example: A parent texted a picture of their child’s scalp at 7:30. I knew this family just had a new baby, and otherwise they’d have to go to urgent care. They lived in my zip code, I had staples at my house, and it wasn’t an inconvenience.
So I said: “Come over, I’ll put in a couple staples, and you can get back to feeding your newborn.”
It was simple.
I didn’t leave my home.
My kids got to watch.
But I told them: “Don’t tell your friends I did this.” That way they knew this was outside the norm. I made clear: this is not the typical experience you should expect.
Step 2: Communicate Boundaries
After deciding internally, you need to communicate boundaries clearly:
Set them with new patients from the start.
With existing patients, explain the reset:
“We’ve let a lot of things slide. Here’s our new system so you get care in the time you need it.”
One of the easiest tools: self-scheduling.
Patients don’t have to wait, text, or call.
You don’t feel guilty and step in because they’ve been waiting.
Instead, you can reply: “To give this the attention it deserves, please book a quick virtual or in-person appointment.”
That way you’re showing: this is worth your time as a parent—and you’re keeping boundaries intact.
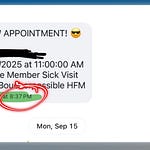
Step 3: Reinforce with Automation
Every time someone texts after hours, they should get an automatic response:
“We’re not open right now. If it can wait, leave it here and we’ll get back to you in the morning. If you need to book an appointment, here’s the link. If you’re deciding whether to go to the ER, here’s the number to call. If it’s an emergency, call 911.”
This does two things:
Sets the expectation so you don’t have to respond personally.
Keeps families from assuming “they usually text me back after hours anyway.”
Now they know exactly what to expect.
Summary
So when it comes to boundaries in pediatric direct care:
Decide on your boundaries.
Communicate them regularly.
Make it easy for patients to respect them.
That’s how you protect your time, energy, and family life while still delivering great care.
👉 Want more conversations like this? Join us at the Pediatric Direct Care Summit at summit.dpcpediatrician.com.